Building Reliable Advances and Innovation in Neurotechnology (BRAIN) Center
June 09, 2020

Healthcare wearables are a booming industry, and many devices have been developed for the elderly to detect falls. But identifying a fall after it has occurred could be too late. Falls are the leading cause of death in older Americans, and for those injured, the medical costs are expected to reach $67.7 billion by the end of 2020, according to the National Council on Aging.
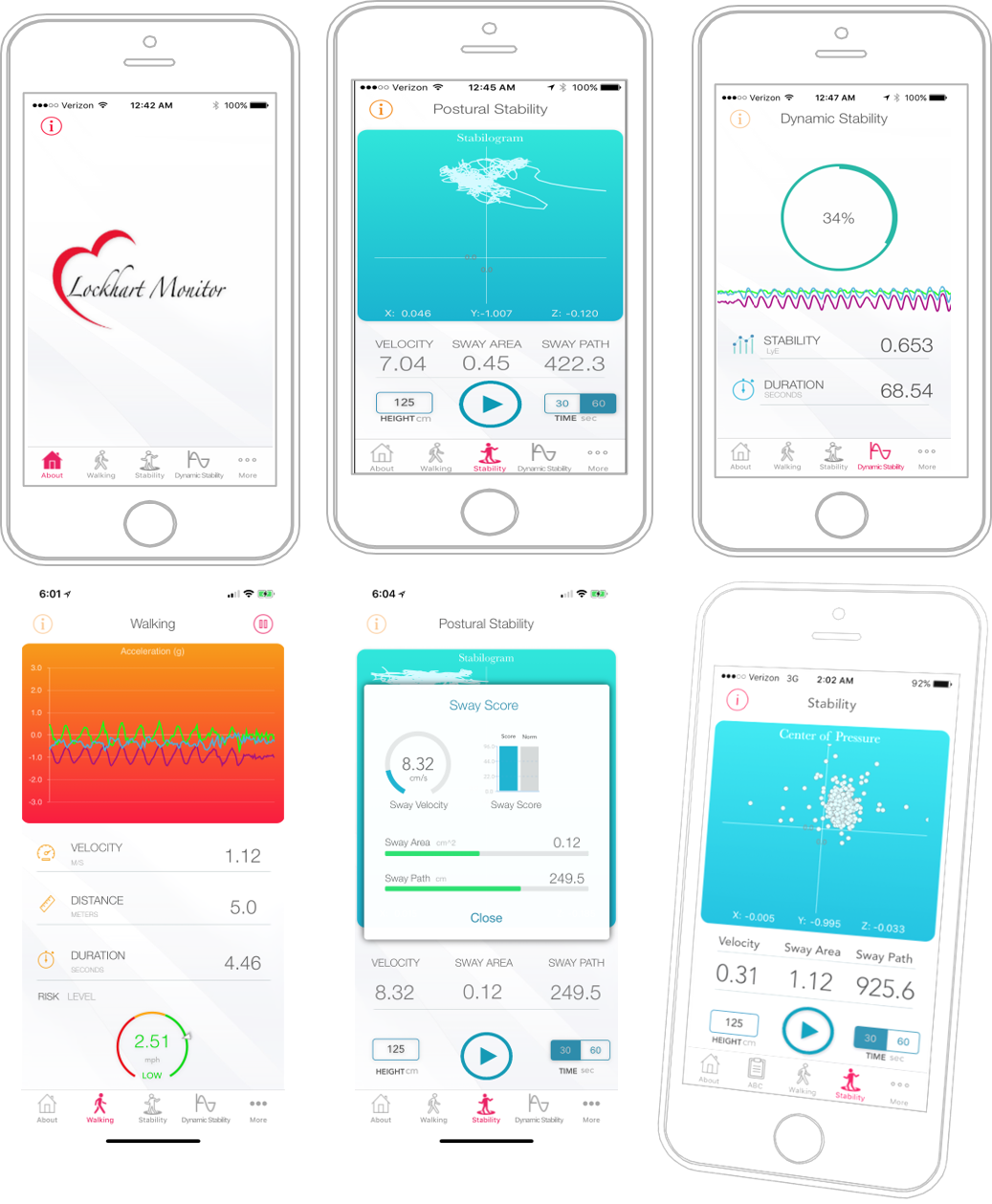
Now for the first time, researchers have developed an app for iPhones that uses the same motion-sensing instruments the phone has for navigation screen orientation to monitor a person’s activity, determine their risk for falling and alert caregivers, if needed. The Lockhart Monitor, developed by biomedical engineer Thurmon Lockhart, a professor at Arizona State University, tracks everyday balance and walking abilities and—in early tests with elderly, orthopedic, and obese patients—accurately predicted fall risks. In an unexpected outcome, Lockhart also found that the app could also be used to monitor a person’s state of mind, he says, because previous studies have shown that the same movements that correlate with fall risk are tightly linked to depression and fatigue.

“Health preservation of our elderly population hinges upon our ability to accurately predict fall risks prior to a fall event and quickly target interventions to improve stability,” says Lockhart, who developed the technology as part of a research collaboration with The Core Institute, an orthopedic and musculoskeletal healthcare facility, an industry partner in the Center for Building Reliable Innovation and Advances in Neurotechnology (BRAIN). This Industry-University Cooperative Research Center (IUCRC) is funded by the National Science Foundation to develop safe, effective and affordable personalized neurotechnologies that diagnose, restore, and enhance mind and body functions.
Lockhart says his own father’s death as the result of a fall inspired him to develop the app. He and his team built the technology for Apple iPhones, which users can wear in a pocket or on a belt clip. As the person goes about their day, their phone’s motion-sensing instruments captures speed and stability data. An algorithm written by the team members and embedded in the app uses data from the sensor to establish a baseline of motion for the user and then track variabilities in gait and posture. When the motion falls outside the normal range, the phone issues an alert in the form of a text message to a designated caregiver.
In 2017, the researchers began testing the app’s underlying algorithm with patients who had undergone joint or back surgery and hip replacements. The team found that people who fell were those who had, perhaps counterintuitively, moved more slowly and showed less variability in their gait and posture than those who didn’t fall. In fact, people who didn’t fall moved more quickly and had more variability in their actions. The researchers didn’t have an explanation for why but follow up studies on people with obesity and osteoporosis showed similar results.
Looking for clues, the scientists read dozens of unrelated published studies that dealt with gait and posture and found the same slow gaits and movements found in people at risk of falling were also found in those with depression and fatigue. “Depression and mobility are closely related, and in assessing such relationships, we are able to determine and quantify this complexity,” says Lockhart. It meant that the researchers could use their phone app to detect not only potential fall risk, but also depression and fatigue. Lockhart says his team is currently planning to validate the cognitive behavioral monitor at a local active-living center for older adults. The study will involve a baseline measure and subsequent daily measures while patients are wearing the mobile phone for up to 100 days, he says.
Lockhart credits the BRAIN Center in large part for his success. “Collaborating with the BRAIN Center not only helped me to validate the device but also helped me to realize what intellectual property was worth commercializing,” he says.
At the moment, the team is currently developing future studies to test the technology on people with depression and they’re also working on specific interventions for post-surgical patients who may be at risk for falling. For instance, in cases where the technology senses that a person’s gait or posture is falling outside of normal range, the app may issue an alert to the patient as well as to a caregiver. Then, depending on the patient’s treatment plan, the app would suggest an exercise or physical therapy intervention to improve the person’s stability.
“In the future, this technology could be wearable and monitor mobility, gait, posture, and physiological indicators or be non-invasive, for instance, be embedded in floors and walls of homes,” says Lockhart.
